One thing everybody wants to know is how and when the Covid-19 pandemic will end. I’m going to try to lay out my understanding of how that can work. Understand that I am not an epidemiologist or healthcare professional. I’m just like everyone else who is trying to understand what’s happening.
This post is basically just my way of thinking out loud about the epidemic. For rather a lot of words. Consider yourself warned.
There’s a funny series of animated videos called How It Should Have Ended, that suggests “better” endings for movies, many of which would have ended the movies a lot sooner. (E.g. Make sure the maintenance doors to the dinosaur pens are too small for dinosaurs to escape.) Well, there’s a way we could have ended the Covid-19 epidemic in the United States a lot sooner.
When the first Covid-19 outbreaks were detected, what we should have done is isolate those people, identify everyone they had come in contact with, tracked them down and tested them, isolated the ones who tested positive, then repeated the process for they had contact with, and so on, until the tracing teams identified and isolated everyone who could possibly spread the disease. Doing this for every outbreak would have stopped Covid-19 in its tracks. Contagious diseases all over the world have been beaten this way.
And we did try to do that. Unfortunately, for various reasons (which should be thoroughly investigated by Congress at some point) there weren’t enough tests available and the process broke down. Soon hospitals — some of which resorted out of expediency to tests that were not FDA-approved — began discovering Covid-19 patients who could not be traced back to any other known cluster of Covid-19 cases. This is called community transmission, and it means that the effort to contain the contagion has failed, and tracking of individual transmission incidents is no longer feasible. The disease had escaped and was going to burn through the population.
That’s where we are now, with Covid-19 now confirmed to have infected over 1.3 million Americans.
To explain what happens next, I’d like to go back to something I skimmed over in my earlier post about a STAT magazine article that mentioned a Covid-19 model by Dandekar and Barbastathis at MIT. It was a compartmental model — in particular, it’s an SIR model — and I’d like to talk about how that model works.
Like all models, compartmental models are simplifications, and the SIR model I’m going to be talking about is nowhere near sophisticated enough to model an actual epidemic. It’s just a tool for thinking about how epidemics work, and I think it will be useful for understanding the past and future of the Covid-19 epidemic.
Compartmental models split the population into compartments and specify mathematical formulas that describe how people move between the compartments. (If you have a computing background like me, you can think of these as states.) The SIR model defines three compartments:
- Susceptible: The pool of people who could catch the disease.
- Infected: The pool of people who currently have the disease.
- Recovered: The pool of people who have recovered and are now immune.
People move through the compartments, starting as susceptible, becoming infected, and then recovering:
Susceptible –> Infected –> Recovered
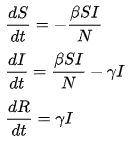
Compartmental models include a set of equations that describe how the number of people in each component changes as the model progresses. For our purposes, I’m going to show you a very simple set of equations from the Wikipedia page on epidemic modeling.
Don’t worry, you don’t have to follow the math. (This is, honestly, at the limits of my memory of differential equations class, which I now regret skimming my way through.) The description that follows will explain the model in plain English (I hope).
To run the model, you specify a few parameters (shown here by the greek letters beta and gamma) which we don’t have to worry about, and you set the starting population numbers S and I to the number of people who are Susceptible and Infected, respectively. If we were to set I to zero, indicating that no one is infected, then all of the derivatives will collapse to zero and nothing will change, which is what you’d expect when no one has the disease. Things don’t get started until someone gets infected. Similarly, if we set S to zero, then there’s no one left to catch the disease, and all that happens is that the infected people in I recover to R.
So in order for something useful to happen, we need people with the disease, and people who can catch it, and as the presence of the term SI implies, the rate at which the infection spreads is proportional to both the number of Infected people and the number of Susceptible people. This captures the common-sense notion that the disease is more likely to spread when a lot of Infected people meet a lot of Susceptible people.
In a typical modeling run, we start with almost everyone in the Susceptible compartment, except for a few Infected people who bring the disease into the population. Each Infected person is assumed to transmit the disease to Susceptible people with some probability, which causes the Susceptible people to move to the Infected compartment.
At the beginning of the epidemic, with the number of Infected people so low, any increase in the size of the Infected compartment produces a proportional increase in the rate at which Susceptible people become Infected, so with even more Infected people, the epidemic spreads even faster, feeding on itself in a period of explosive expansion. This is called exponential growth, and it has some scary implications.
The rate at which each infected person infects other people is denoted by the reproduction number R0. If R0 =2, for example, then each Infected person can infect two Susceptible people, and each of those new Infected people can infect two more Susceptible people, and so on. If we assume people are infectious for an average of one week, a single infected person can lead to a pandemic that infects everyone on Earth in 33 weeks. It’s a real doomsday scenario.
(Note: I’m using figures like R0 =2 and a period of 1 week to keep this example simple. These are not based on actual figures for Covid-19.)
Fortunately, the doomsday scenario is not a realistic scenario, because in order for an Infected person to transmit the disease to a Susceptible person, they have to encounter a Susceptible person, but as Susceptible people are infected, they move to the Infected compartment, and the Susceptible compartment shrinks, reducing the probability that each Infected person can infect a Susceptible person. This makes it less and less likely that Infected people will transmit the disease to Susceptible people, effectively reducing the reproduction number R0 to some lower effective reproduction number Re.
Initially, a disease might have Re = R0 = 2, meaning each Infected person would transmit the disease to two Susceptible people, and so on, for a period that resembles exponential growth. However, when 10% of the population has been Infected (or Recovered), that means 10% of those disease transmissions are wasted on people who cannot be infected, effectively lowering Re by 10% to 1.8, so that each infected person can only infect 1.8 other people per week. The more the Susceptible pool shrinks, the lower Re gets, and slower the rate of new infections grows.
Eventually, as the pool of Susceptible people gets small enough, Re will fall below 1, meaning that Infected people are no longer guaranteed to replace themselves before they transition to the Recovered compartment. The rate of infection stops increasing — i.e. it reaches its peak — and then begins to decrease as the pool of Susceptible people dwindles further. At some point, the shrinkage of the Susceptible pool causes the epidemic to slow down so much that all the Infected people recover recover before any new Susceptible person is infected, letting I reach 0, which means that everything stops changing, and the epidemic ends.
(You may be wondering where people who die fit into this model. To keep things simple, they are usually lumped in with Recovered people since, like Recovered people, they can neither be infected nor infect someone else. That’s why the equations above have no R terms on the right-hand side — the Recovered people have no direct effect on the dynamics of the epidemic. Because of this, some descriptions of the SIR model refer to the R group as Removed instead of Recovered.)
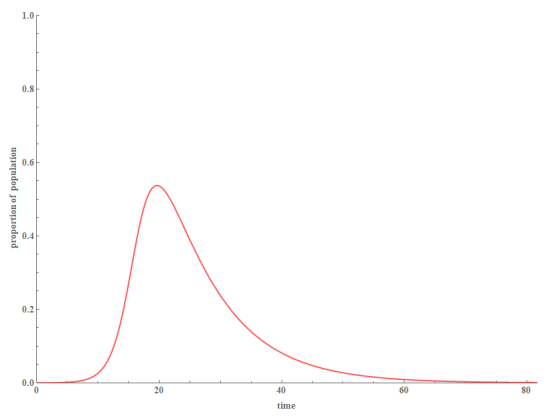
Graphically, the timeline for this scenario in a typical SIR model would look something like this (with Susceptible people in blue, Infected people in red, and Recovered people in green):
(The numbers on the graph are illustrative only, and have no relationship to the numbers in the description above or to the actual Covid-19 epidemic.)
If that seems too simple, you’re right. There are many variations on compartmental models that take into account complicating factors such as delays between infection and contagiousness, reinfections, births, deaths by other causes, multiple groups of people, migrations, interventions, and so on. The flexibility of the compartmental model framework is one of the things that make these models so useful.
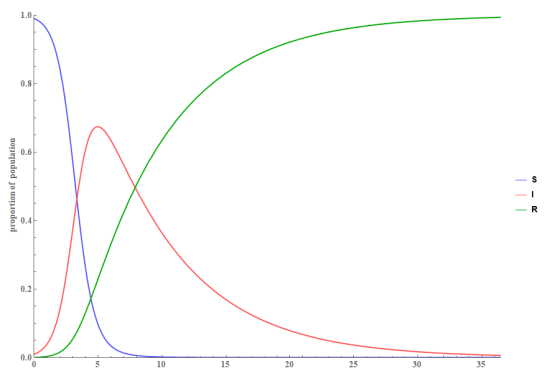
One of the goals of our current policy is to “flatten the curve” by implementing a “lockdown” — using social distancing, masks, shutdowns of many businesses, cancellations of large gatherings, and so on. This should reduce R0, thus reducing the rate at which Susceptible people enter the Infected compartment, without reducing the rate at which Infected people move to the Recovered compartment, thus reducing the number of people in the Infected compartment at any one time. This, in turn, prevents the epidemic from overwhelming the hospital system, as happened in Lombardy, Italy. Flattening the curve might look something like this:
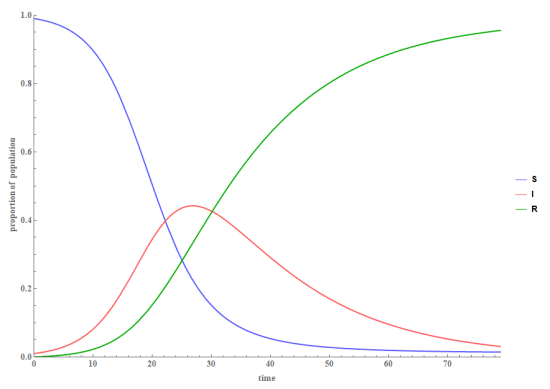 Basically, the reduced R0 causes the whole process to slow down and take longer, which reduces the height of the Infected peak. (The height of the peak shown here is unrealistically high — over 40% — especially for a large population like the U.S., and is for illustration purposes only.)
Basically, the reduced R0 causes the whole process to slow down and take longer, which reduces the height of the Infected peak. (The height of the peak shown here is unrealistically high — over 40% — especially for a large population like the U.S., and is for illustration purposes only.)
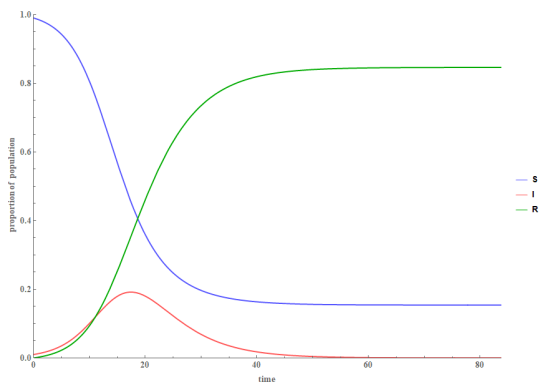
Under the right conditions, the natural R0 of a disease may be low enough that the reduction in the size of the Susceptible pool slows down the spread of the infection so much that all the people in the Infected pool recover before the entire Susceptible group is infected. That produces a result that looks like this, where the infection is over even though almost 20% of the population is still Susceptible.
That’s because under the modeling parameters that I used for this graph, R0 is so low that when the Susceptible pool is smaller than about 20%, Re is forced low enough below 1 to eliminate the infection.
This is sometimes referred to as herd immunity, because even though individual people in the Susceptible compartment can still catch the disease if exposed, they are unlikely to be exposed because even if some new Infected people are re-introduced to the population — e.g. travelers from a region where the infection is still active — the same factors that stopped the first outbreak will quickly eliminate the new outbreak as well. Thus while some individuals are susceptible to the infectious disease, the collective population — the herd — is effectively immune.
Some people argue that our best strategy for dealing with the Covid-19 epidemic is to lift the lockdown and let the virus spread until we reach herd immunity, which they estimate might happen when the Susceptible population drops to about 30%. They argue that (1) the economic cost of the lockdown is too high to remain locked down for very long, and (2) unless we are willing to remain locked down for the one or more years it will take to get a vaccine, we will all get infected to the point of herd immunity anyway, so we might as well do it quickly to minimize the economic pain.
I believe this is misguided for several reasons:
- Covid-19 has a non-trivial fatality rate, and allowing 70% of Americans to be infected by it will result in a large number of deaths.
- Even when it doesn’t kill, Covid-19 is a hard disease, and many people will suffer from it. We are learning that some Covid-19 patients develop life-long disabilities.
- Flattening the curve reduces the risk of overwhelming our healthcare capacity, thus increasing the cost in lives and suffering.
- Slowing the spread of the disease gives our healthcare industry more time to learn about the disease, more time to find innovative solutions, and more time to prepare a response, thus reducing the harm from the disease.
I can’t let this go without mentioning that some loathsome people are making the argument that previous generations — World War II veterans, the Greatest Generation — were bravely willing to make the ultimate sacrifice to preserve our way of life, and therefore we should be equally brave and willing to sacrifice…the lives of other people, who we will let die from Covid-19, to preserve our economy. And anyone who refuses to do this is a coward who spits on his ancestors’ memory. (I exaggerate only slightly.)
Seriously, just how messed up do you have to be to think that making economic sacrifices to save American lives is the cowardly move here? If these people really want to show they are bravely willing to help Americans, they should volunteer to be deliberately infected with the SARS-Cov-2 virus to speed up vaccine trials.
Note that I am not dismissing any arguments about “opening up” the economy as sacrificing lives for money. For one thing, it’s better described as risking lives for economic well-being. That is, doing something to improve the quality of life, at the risk of loss of life. People have been making high-stakes decisions like that throughout history — from refugees crossing dangerous waters, to people working at hazardous jobs because they pay well, to consumers who buy smaller cars to save the money for something else. I regard making these kinds of decisions about our own lives as a fundamental right.
Economist Steven E. Landsburg illustrated this concept by asking a question something like “Would you press a button that would prevent a billion migraine headaches if it also killed one person?” He answered that he would, because one life is a small price to pay to prevent so much suffering. That shocked me the first time I read it — he can’t be serious, can he?
But then I thought about it a little and came up with a different way to ask almost the same question: You’ve got a migraine headache, and there’s a new pill on the market that will stop it in 15 minutes. Would you take that pill if there was a 1-in-a-billion chance it would kill you? I’m pretty sure a lot of people would, just as many people take dangerous jobs to make more money. And if people are demonstrably willing to risk the length of their lives to improve the quality of their lives, then there’s an argument to be made that public policy should reflect their choices and try to reach a similar balance between those goals.
However, there are three points I think are important:
- There’s an ugly history of public policy that is far too cautious, adding great cost and inconvenience for little benefit.
- There’s an even uglier history of public policy that regards human lives as disposable.
- The best public policy lets people make their own decisions about their own lives.
Nevertheless, while agreeing in principle that a poor economy also costs lives and causes suffering, I haven’t seen compelling calculations that convince me we’re committing “economic suicide.”
And there is a better way, which I alluded to earlier, and will get back to in a moment.
There’s no denying that much of the current “lockdown” was hurried and poorly planned, with rules that seem wildly inconsistent, and that are too strict in some ways, preventing people and businesses from coming up with flexible responses. That’s always a potential problem with laws and regulations, but the hurried nature of the emergency makes it worse, and the stakes are even higher than normal.
There’s also no denying that a lot of Americans are in financial trouble right now, especially since the lockdown period is dragging on much longer than many people expected. We’ve all seen the protests, and while the assholes get all the attention, there are a lot of people who are simply desperate for the lockdown to end.
The problem is, the lockdown is really more of a “hunker down.” Evidence from data sets like centralized restaurant reservation systems, the travel industry, and GPS tracking of mobile phones shows that much of the change in public behavior came independently of government lockdown orders, which means that lifting the lockdown orders may not do much to restore economic activity. Customers just aren’t going to return to businesses they don’t think are safe.
Simply put, to open up the economy, we have to make economic activity safe.
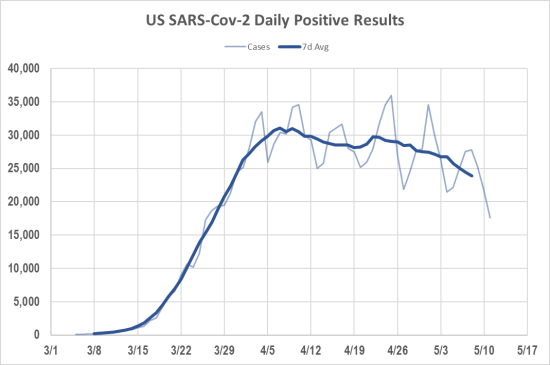
That brings me right back to the SIR model. By taking all these actions — shutting down schools and businesses, social distancing, wearing masks, washing our hands — we are trying to reduce the probability of transmission of the Covid-19 virus, which will reduce the base reproduction number R0 of the virus. If we can get R0 to be less than 1, then the effective reproduction number Re also has to be less than 1, which will make the epidemic die out. It should cause the Infected compartment to follow that familiar curve we’ve been seeing everywhere:
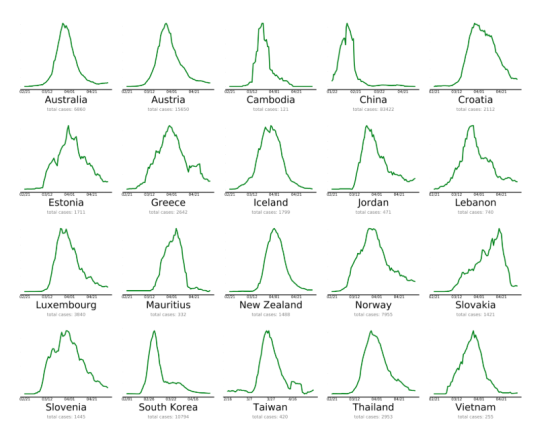
With 25,000 new cases per day in the U.S. right now, suppressing the curve this way may seem unrealistic. But it’s completely doable. Here’s proof:
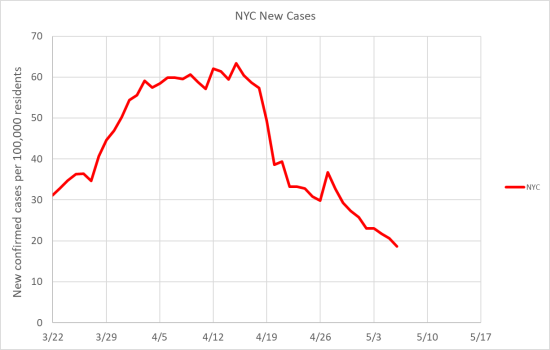
If those other countries can do it, there’s no good reason we can’t. (You can check how the U.S. and other countries are doing at EndCoronavirus.org) Here in the U.S., New York City seems to be making good progress. They’ve been through hell, but it looks like they’re making their way back:
So this is totally possible. But the U.S. still has some work to do:
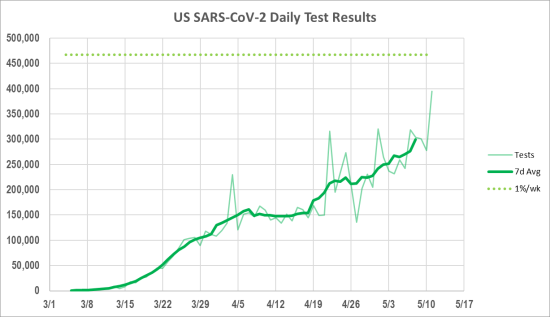
We seem to be stuck on a gently sloping plateau. I think this is partly because the U.S. is big enough for the epidemic to be running on different timelines in different places, so while New York City is coming down, other parts of the country are still rising. I also think that the recent increase in the availability of testing is responsible for at least some the apparent rise in cases in some parts of the U.S. That is, the cases were always there, they just weren’t being picked up until we had more tests.
Once the number of cases drops a lot closer to zero, many kinds of economic activity will become relatively safe again. However, if we go right back to the way things were at the beginning of the epidemic…we will find ourselves at the beginning of another epidemic. We’ll trigger a second wave, and the economic sacrifices we’ve made to fight the first wave will have been for nothing.
We can’t let that happen.
The solution is a return to Plan A: Test, trace, and isolate. This failed the first time, because we weren’t ready and didn’t have enough tests. On March 1, we were doing fewer than 1000 tests per day. We’re now up to over 300,000 tests per day, and that’s expected to grow as more testing capacity comes online.
I’ve seen several different estimates of the number of tests we’ll need to begin opening up again — among other things, it depends on what you mean by “opening up.” The Rockefeller Foundation’s plan recommended testing about 3 million tests/week to reach the next phase, and the folks at Covid Exit Strategy are tracking a target of 500,000 tests per day. Since both of those are around 1% of the U.S. population, I’ve been tracking that as my target. (Shown by the dashed green line above.)
Testing 1% of the U.S. population per week may not sound like much — it would take almost two years to test the entire population. But we don’t need to test the entire population to begin making some safe changes. At that level of testing — assuming the epidemic curves down according to plan — we should have enough testing capacity for hospitals to diagnose patients with respiratory illnesses (which until recently accounted for most testing) while still making tests available to community medical providers and allowing us to effectively screen key personnel, such as hospital staff and transit workers.
With low infection rates, that level of testing should also allow us to have contact tracing teams investigate new Covid-19 cases, find out who the infected person has been in contact with, and get everybody tested. Infected individuals can then be quarantined, ideally in special-purpose isolation facilities, rather than at home where there’s a chance they’ll infect members of their family.
In terms of the SIR model, isolation of people who test positive is the equivalent of creating a model with only a single person, who happens to be in the Infected compartment. Without any Susceptible people around, the only allowed transition is for the Infected person to move to the Recovered compartment (or Removed, if they die). No one else gets infected.
South Korea did a terrific job of test-and-trace when Covid-19 first hit. Despite discovering their first infections at the same time the U.S. did, they’ve only had 11,000 cases and 260 deaths in a population of 50 million. They’ve begun opening up, but they just had a setback when some guy visited a bunch of nightclubs and then tested positive for Covid-19. South Korean health authorities have closed all the clubs, and tested 2400 of the 5500 people who were potentially exposed, identifying 80 cases so far, including 35 in a single day, which is the highest single-day number of new Covid-19 cases in South Korea in the last month.
Imagine how great it would be in the United States if 35 cases in a single day was big news.
Fortunately, opening up the economy and maintaining good infection control aren’t entirely mutually exclusive. There are certainly some activities that will be difficult to do safely, especially those involving close contact or large numbers of people, but I think we can make many things safer with a little ingenuity.
We mostly know what it takes to stop infections from spreading — masks, gloves, gowns, washing hands, cleaning surfaces — and we already have a lot of the basic technology in our healthcare industry. It’s true that a lot of healthcare workers have caught the virus, but given that they are spending so much time in close proximity to people who very definitely have Covid-19, it’s not as many as you might think. There’s even some evidence that infection rates are lower in some healthcare workers than in the general public they serve.
If nurses can figure out how to safely take vitals and draw blood from Covid-19 patients, we can probably figure out protocols to safely cut someone’s hair or sell them retail goods. This will require a massive increase in production of personal protective equipment (PPE), but that’s happening anyway, and healthcare workers won’t need so much of it if we can keep the epidemic small.
We’ll also probably need to develop PPE that is specific to our purposes. Doctors and nurses need to switch out their PPE every time they switch patients, to avoid spreading infections. But in the relatively low-risk environment the rest of us face, that is less likely to be a concern. We might do better with PPE designed for easier fit, comfort, and long-term wear, perhaps even with the possibility of sterilization and cleaning.
It won’t be perfect, but it doesn’t need to be. Anything that helps reduce the probability of transmission can help keep R0 down.
It’s possible that we will never entirely defeat Covid-19. There are ancient killers still among us, like leprosy, mentioned in the bible, or tuberculosis, which has left signs of infection in the fossilized remains of people who died half a million years ago. Leprosy is largely survivable these days, but tuberculosis still kills about 1.5 million people a year.
We’ve had some successes at eradicating diseases. Smallpox has been wiped out for decades, and two of the three known strains of polio have been eradicated, with the remaining strain thought likely to disappear as well. Malaria has been wiped out in much of the developed world, and may be eradicated from a few remaining stronghold regions in another couple of decades.
Some diseases hide in animal hosts. Ebola has been eliminated from the human population multiple times, only to spring up again when a human somewhere catches a case from whichever animal species is serving as a reservoir. (Bats are a key suspect.) Rabies circulates in mammal populations, and is transferred to humans by a bite, but human-to-human transmission is all but non-existent.
On the other hand, influenza viruses have survived all attempts to eradicate them from the human population. The flu is a modern disease, successful at persisting in the human population because we insist on living close together in giant cities. And it mutates quickly enough that even our vaccines cannot keep up with the changes. The Spanish flu may be gone, but its related H1N1 family of viruses is still killing people.
Fortunately, many of the diseases that survive in the human population have evolved into milder forms. Diseases that kill quickly don’t leave themselves much time to spread, so mutations that leave their hosts alive and mobile are more likely to survive and thrive. We all catch one or another of the 160 identified rhinoviruses several times a year, and we treat them with over-the-counter cold medicine.
Unfortunately, even viruses don’t evolve quickly enough for this to help us right now.
Fortunately, there may be a magic bullet: A vaccine. Last I heard, over 90 labs are trying to develop a vaccine, and 9 of them have begun Phase 1 trials for safety. We’ve never developed a vaccine for a coronavirus in humans before, but we have several for livestock, and experts expect we will be able to make one for SARS-CoV-2 as well. The 12-18 month figure that everyone throws around would probably be the earliest, and it may be optimistic — most vaccines take longer.
When we got hit with the first SARS virus at the beginning of the century, a program was launched to develop a vaccine, but SARS was less contagious than SARS-CoV-2, and it was eliminated in 2004 through the kinds of social distancing and testing measures I outlined above. At that point, vaccine development was abandoned, but scientists learned a thing or two about how to make a vaccine for this type of virus. Also, we’ve gotten super-good at genetic tinkering these days.
In terms of the SIR model, a vaccine works by conferring immunity to a disease on people who’ve never had it, effectively moving people from the Susceptible compartment to Recovered, without ever having to go through the Infected state. This lowers Re, ideally well below 1, resulting in herd immunity without the need for people to catch the disease or die.
So, that’s the plan: (1) Hunker down now to suppress the outbreak to manageable levels, (2) limit the spread with infection control measures, (3) manage the outbreak with testing, tracing, and isolation, and (4) develop a vaccine.
I hope we’re smart enough, industrious enough, and good enough to make it work.
Excellent article. You explained things in terms that even I can understand. Bravo.
Heh. Thanks for stopping by, Chris.
There’s been a lot of debate about the steps we’re taking, or should be taking, to stop Covid-19, but I haven’t seen anything that pulls it all together to explain the whole public health plan, so I’ve tried to put something together based on all the things I’ve read. I included the SIR model because I found it to be a useful mental tool for explaining what’s happening, and what we are hoping to accomplish with all this social-distancing/lockdown effort, and why we believe it could work.
Also, I particularly wanted to address the “we can’t just lock down until the vaccine” argument by explaining that that’s not the plan. We can (probably) beat this thing, or at least greatly reduce the threat, without having a vaccine. SARS, MERS, and Ebola outbreaks have all been beaten that way in the past.